
Location
Nuffield Orthopaedic Centre, Oxford, OX3 7LD
Biography
Tom Cosker is a Consultant Orthopaedic Surgeon, who gained his Completion of Specialist Training in 2011. He works at the Tumour Oncology Unit in the Nuffield Orthopaedic Centre, Oxford and has a specialist interest in Upper Limb Surgery and Reconstruction. He is Upper Limb Fellowship trained and completed a Fellowship at the Princess Elizabeth Orthopaedic Centre in Exeter under the mentorship of Professor Tim Bunker.
Tom has previously worked at Stoke Mandeville Hospital (Spinal Injuries, alongside some of the UK’s foremost spinal surgeons), High Wycombe Hospital (specialising in Arthroplasty and general orthopaedic trauma), Royal Berkshire Hospital (specialising in Upper Limb Surgery) and the John Radcliffe Hospital (specialising in General Orthopaedic Trauma).
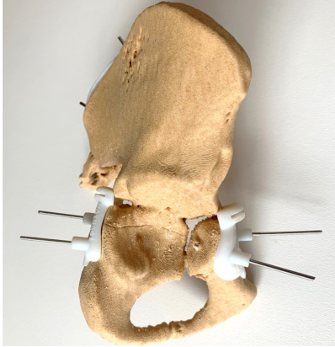
Examples of 3d printed models and tumour cutting guide to allow safe resection

Thomas Cosker
MB BCh FRCS (Tr & Orth) MSc FAS
Associate Professor
- Director of Surgical Anatomy
- Consultant Orthopaedic Oncology Surgeon
As Director of Surgical Anatomy, I am responsible for delivering anatomy training to clinical medical students, post-graduate junior surgeons preparing for the MRCS, and in the new Oxford Surgical Training Centre we will be delivering “cradle-to-grave” learning at various levels for more experienced surgeons across the range of surgical specialties. I have an active research programme with grant funding raised from NOHF and Bone Cancer Research Trust.
Our work has been presented and acclaimed nationally and internationally. I am Clinical Lead for Sarcoma Surgery at OUH. I am the Surgeon Designer for a new Hip, Knee and Shoulder replacement system with Adler Orthopaedics and have secured financial support for world class research at our labs in Oxford. I opened the first dedicated 3D printing lab in a new facility at the Nuffield Orthopaedic Centre which has worked as a collaboration between the NHS, University of Oxford and Industry (3D Life Prints).
The 3D printing lab has used state of the art 3d printing technology to take encrypted in vivo CT and MRI data from real patients, translate this into digital files, pass it through a medical artist and then print high definition 3d printed models for use in teaching and in surgery. We are creating the Oxford Library of Anatomy and have already printed models for the retroperitoneum, the urinary tract, the hepatobiliary system, the brachial plexus, the pelvis and the base of skull. Our work has been published (see below) extensively and presented at international meetings. We are currently finalising our model of the mediastinum. The models are also now being translated into practical use with printed jigs to assist with tumour resection and this has the potential to revolutionise tumour surgery worldwide. It is envisaged that with the creation of the new Oxford Surgical Training Centre, the lab will be embedded in a new facility and increase in size.
I am an author of 36 journal articles, 22 conference proceedings and a book chapter. I am first author on five journal articles and senior (last) author on twelve publications. My last first author publication was published in 2014 and the articles on which I am senior author were all published in the last four years. After 2015 in my role as Director of Human Anatomy and now Director of Surgical Anatomy, my oversight changed to reflect my position as the Director. Since 2015 I have been responsible for creating and supervising projects rather than carrying them out under supervision.
Having worked for six years as Director of Human Anatomy for DPAG, I am delighted to have been appointed as Director of Surgical Anatomy at NDS where I have assumed responsibility for surgical teaching to University of Oxford clinical medical students, post qualification junior surgeons and in the future training of more senior surgeons in the Oxford Surgical Training Centre. I have developed the principle of “cradle to grave surgical teaching” to emphasise the belief that teaching should not occur as a snap-shot in time but rather an experience which accompanies trainees from their first day at medical school to higher level surgical teaching as they attend masterclasses in their chosen specialty.
I have acted as Examiner at BM1 for three years, Chief Examiner for PCA for three years, served on the BM1 Teaching Committee for seven years, served on the PCA teaching committee for seven years, ran the DPAG Anatomy Committee for seven years and am now part of the NDS planning meetings.
I am currently involved in a high-level proposal between the Medical Sciences Division and Oxford University Hospitals NHS Foundation Trust (OUHFT) to establish a new international centre of excellence in surgical teaching, simulation, and training: The Oxford Surgical Training Centre (OSTC). Changes in training and new surgical techniques require novel methods to not only enthuse and support our future surgeons, anaesthetists, nurses, midwives, and theatre staff, but also support the lifelong learning of our consultants and matrons.
The new facility will be a state-of-the-art, multidisciplinary, education centre which will draw on the latest technological innovations to offer high fidelity procedural training in surgical and allied disciplines across all specialties.
The OSTC would further showcase the close partnership between the Nuffield Department of Surgical Sciences (NDS), Oxford University Hospitals NHS Foundation Trust (OUHFT), Oxford Medical School, and Health Education England Thames Valley (HEETV). Specifically, when fully operational, the centre will conduct over 100 courses per year for medical students, surgical trainees and consultants, anaesthetic trainees and consultants, nursing and midwifery students, and theatre staff. This will place Oxford at the centre of the South East’s recruitment and retention of theatre staff, and will contribute to building stronger and safer surgical teams providing better patient care.
Recent publications
-
Nomogram Predicting the Risk of Postoperative Major Wound Complication in Soft Tissue Sarcoma of the Trunk and Extremities after Preoperative Radiotherapy.
Journal article
Ouyang Z. et al, (2022), Cancers (Basel), 14
-
Surgical Outcome and Oncological Survival of Osteofibrous Dysplasia-Like and Classic Adamantinomas: An International Multicenter Study of 318 Cases.
Journal article
Schutgens EM. et al, (2020), J Bone Joint Surg Am, 102, 1703 - 1713
-
Patient safety associated with the surgical treatment of bone and soft tissue tumours during the COVID-19 pandemic-results from an observational study at the Oxford Sarcoma Service.
Journal article
Rajasekaran RB. et al, (2020), Int Orthop, 44, 1853 - 1858
-
Surgical Outcome and Oncological Survival of Osteofibrous Dysplasia-Like and Classic Adamantinomas: An International Multicenter Study of 318 Cases.
Journal article
Schutgens EM. et al, (2020), J Bone Joint Surg Am
-
Service delivery during the COVID-19 pandemic: Experience from The Oxford Bone Tumour and Soft Tissue Sarcoma service.
Journal article
Rajasekaran RB. et al, (2020), J Clin Orthop Trauma, 11, S419 - S422

